Posted on: February 15, 2021
COVID-19 has overwhelmed health systems worldwide, leading to worrisome drops in essential health services for preventable, yet deadly diseases. Many facilities in Kenya and Uganda are overstretched and understocked, and travel restrictions and fears of leaving home are keeping some from seeking essential preventative, routine and even urgent care. A recent review of government data in Kenya and Uganda revealed up to 35% declines in the number of people who sought facility-based care and treatments for common childhood diseases such as malaria, diarrhea and pneumonia due to COVID-19.
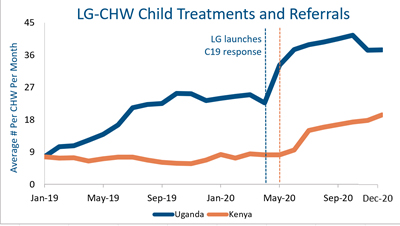
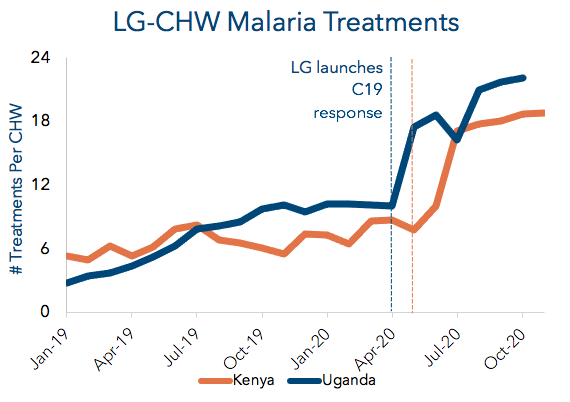
In contrast to these national trends, treatments for these same diseases in our direct operations have nearly doubled in areas where Living Goods supports government CHWs. These CHWs are surpassing expectations on many fronts, supported both by the strong community health platform Living Goods had in place pre-pandemic along with the numerous programmatic adjustments we made in response to it. Household demand for CHW services increased significantly due to the travel-restrictions, fear of facilities and economic hardship brought on by COVID-19, and several of the adjustments we designed were intended to drive more equitable care. CHWs, in turn, were able to fill vital gaps in essential health service delivery and meet the increased demand of neighbor families who felt safer visiting them and motivated by the free services and education CHWs were offering.
Here’s a sampling of the results achieved by CHWs in Living Goods’ direct operations in 2020:
As noted above, families increasingly turned to CHWs for health care during the crisis, both given their increased difficulties and fears around visiting facilities and because Living Goods removed some key barriers to care to ensure health service continuity. Key elements of our COVID-19 response included free essential medicines, a revised CHW compensation structure, remote supervision, and adjusted digital health workflows.
MALARIA: CHW treatments or referrals increased 99% in Kenya’s malaria-endemic areas and soared 138% in Uganda.
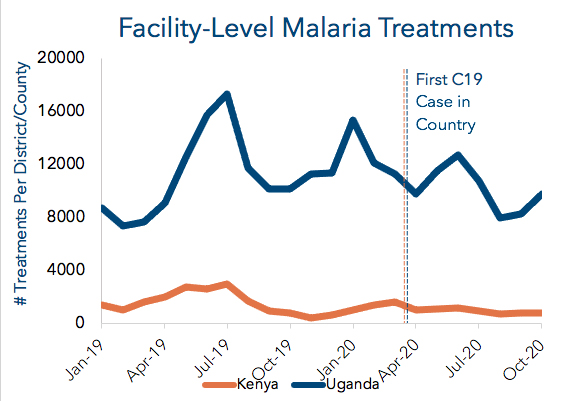
Malaria is also a pandemic and represented 16% of outpatient visits in Kenya and 34% in Uganda pre-COVID-19. Governments made massive strides in combatting malaria since 2000, but we feared the gains in malaria treatment might be undone by COVID-19, as modeled in The Lancet. Our analysis of DHIS2 data shows that in the areas where we work, malaria treatments at health facilities dropped 35% in Kenya and 1% in Uganda from 2019 to 2020. Some overtreatment of malaria was likely captured in Living Goods’ Uganda results due to a temporary policy of presumptive diagnosis for part of the year. This may account for about 30% of the increase in malaria cases recorded, but it has been accounted for in our lives saved estimate. We have since transitioned back to confirming the disease via mRDTs, in line with national COVID-19 protocols.
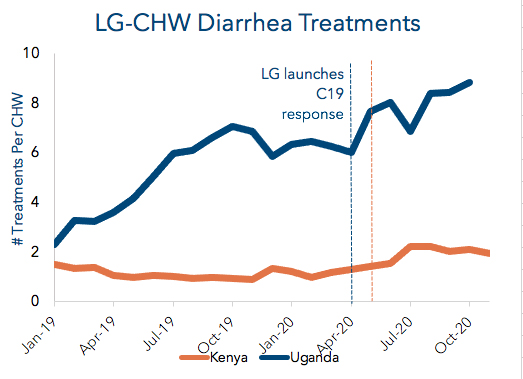
DIARRHEA: CHW treatments or referrals increased 46% in Uganda and 48% in Kenya in 2020.
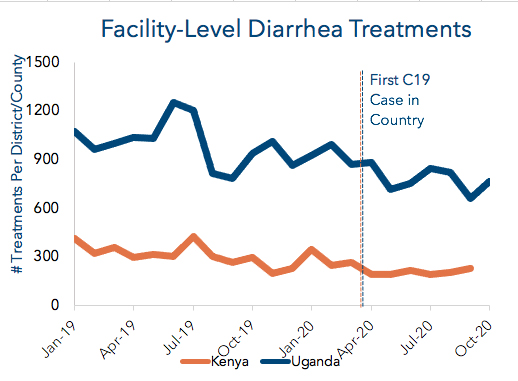
Diarrheal disease is the second leading cause of deaths of children under age 5 (U5) globally but is both highly preventable and treatable. CHWs play an essential role in reinforcing messages about hygiene and sanitation while simultaneously providing families with inexpensive, life-saving treatments like zinc and oral rehydration salts. DHIS2 data of facility care where we operate shows that diarrhea treatments fell 18% in Uganda and 25% in Kenya from 2019 to 2020.